Nursing Pilot Projects Tackle Issues in Rural Health
The Center for Nursing Science and Innovation at Duke University School of Nursing has granted funding for three faculty-led pilot projects that will support health equity in rural settings, from substance use care to surgery.
The School of Nursing’s Ruby L. Wilson Center for Nursing Science and Innovation selected three faculty studies for the Spring 2025 Pilot Research Award, granting them funding for a period of 18 months to kickstart projects that will inform equitable and effective healthcare solutions across North Carolina and beyond.
“We are thrilled to support these innovative pilot research projects that reflect the CNR’s commitment to improve health outcomes in individuals, families, and communities facing health challenges that are made exponentially more difficult because of health inequities,” said Sharron L. Docherty, PhD, RN, PNP, FAAN, Associate Professor and Vice Dean for Research. “These grants empower our DUSON scientists to explore bold ideas, generate preliminary data, and lay the groundwork for future large-scale studies that will shape the future of healthcare.”
“These grant awards will support the groundbreaking work of three teams of investigators in areas where critical health disparities are being experienced in rural and underserved communities,” Dr. Docherty continued. “From mapping systemic barriers in substance use care to understanding surgical experiences among older Black adults, and tackling stigma in opioid use disorder treatment, these projects exemplify the power of nursing research to drive meaningful change.”
Spring 2025 Pilot Research Award-Winning Projects
“The Use of Systems Mapping to Identify Barriers, Redundancies, and Gaps in Rural Health Services Related to Substance Use Prevention/Treatment/Recovery”
Devon Noonan, PhD, MPH, FNP-BC, CARN, FAAN, Associate Professor, Associate Dean of Community Engaged Science, and Director of Rural Health Equity for CNR, is partnering with Marissa Abram, PhD, PMHNP-BC, CARN-AP, FIAAN, Assistant Professor, to conduct a mixed-methods systems mapping study co-led by their rural community partners in Edgecombe County.
“To effectively address substance use in rural settings, it’s essential to understand the complex, multilevel factors shaping prevention, treatment, and recovery,” said Dr. Abram. “Our team has been working in Edgecombe County—a medically underserved, predominantly rural area—using photovoice methods to explore lived experiences with substance use and systemic barriers to care.”
Photovoice is a research method that has study participants capture photographs from their own experiences, which are then used to facilitate group discussions. According to Drs. Noonan and Abram, these discussions helped identify barriers that were impeding access to health services, while also highlighting factors that contributed to resilience. Now, through further focus groups, interviews, and surveys, they hope to lay the foundation for a systems-level intervention to support those struggling with substance use.
“This project will generate critical insights to guide public health strategies, policymaking, and future research,” said Dr. Noonan. “By integrating both traditional (clinics, hospitals) and non-traditional (schools, churches, CBOs) entities identified by community members, we aim to co-design a holistic, integrated care model that emphasizes equity, community resilience, and local governance—all of which are critical to sustainable substance use prevention and recovery in rural communities.”
“Understanding Peri-Anesthesia Care Experiences for Common Nonemergency Surgery Among Older Black Individuals in Rural North Carolina”
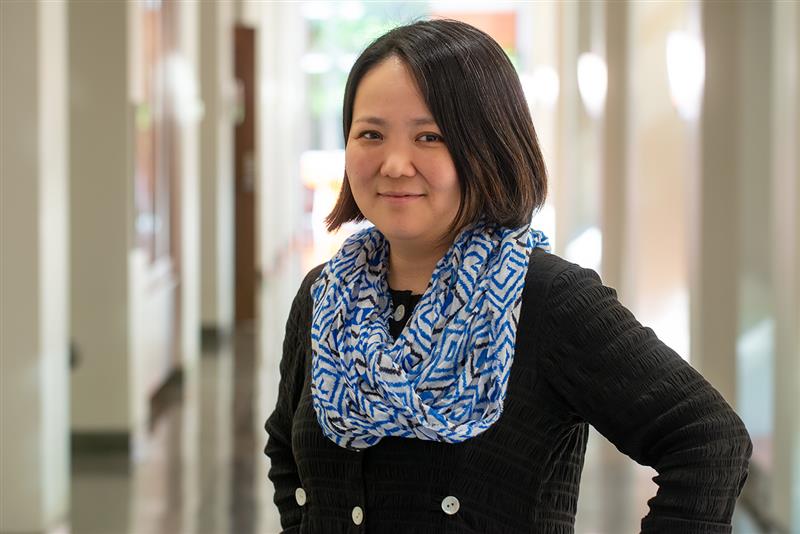
Hideyo Tsumura, PhD, DNP, RN, CRNA, Assistant Professor, will conduct a mixed-methods study exploring peri-anesthesia experiences among older Black individuals in rural North Carolina, who face significantly higher postoperative mortality and complications compared to their white counterparts. Through narrative interviews and surveys, she and her co-investigator, Associate Professor Eleanor McConnell, PhD, MSN, RN, BC, aim to understand and develop an intervention to mitigate these disparities.
“My clinical experience as a nurse anesthetist has provided invaluable insight into these challenges faced by older Black patients living in rural communities,” said Dr. Tsumura. “Many older adults from rural areas drive hours to undergo surgical procedures, often facing obstacles that compound their access to equitable health care. This inspired me to delve deeper into the intersection of rurality and racial and ethnic disparities in healthcare, further fueling my passion for addressing these inequities.”
Dr. Tsumura intends for this pilot study to lay the groundwork for meaningful change. “Our findings will form a foundation of a submission proposal for external funding to develop and test an intervention study designed to improve these care experiences,” said Dr. Tsumura.
“Addressing Multi-level Stigma Towards Opioid Use Disorder in Clinic Practices: Adaptation of the Total Facility Approach for North Carolina Healthcare Systems”
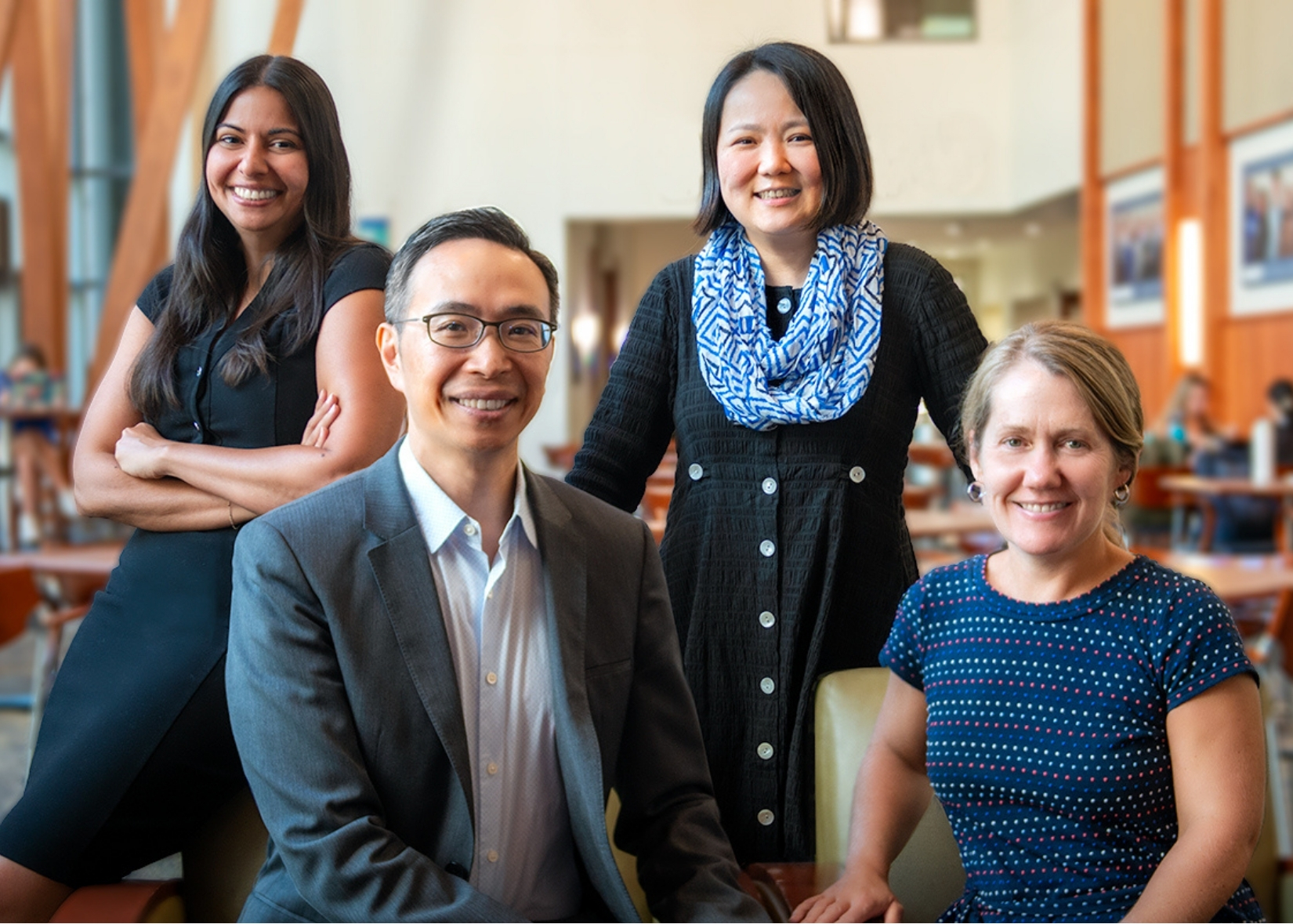
Lawrence Yang, PhD, Pauline Gratz Distinguished Professor, is co-leading this project with Dr. Marissa Abram to adapt the evidence-based Total Facility Approach (TFA) intervention, originally developed for HIV stigma, to address multi-level stigma toward opioid use disorder (OUD) within rural North Carolina healthcare systems. This project will also be conducted in partnership with Dr. Devon Noonan and Margaux Grivel, PhD, Associate in Research. TFA uses a three-stage approach that involves conducting research within a given facility, training healthcare personnel to recognize and address stigma, and integrating locally developed solutions into existing structures and processes. Tailoring this intervention specifically to OUD, Dr. Yang and his team hope to lay the groundwork for nurse-led opioid stigma reduction.
“This work builds on our team’s prior work on OUD stigma and multi-level stigma interventions in diverse populations,” said Dr. Yang. “Building on this expertise, we will adapt the TFA for OUD and integrate it into a nurse-led framework tailored to rural North Carolina, providing a novel and scalable approach to reducing stigma at the level of clinic-level practices and processes.”
The project intends to “leverage nurses as core agents of change within primary care” and to create a useful model that other clinics and practitioners can build upon.
“We aim to develop an adapted intervention package that is feasible, acceptable, and ready for larger-scale optimization testing,” Dr. Yang added. “Ultimately, this study will inform strategies to reduce multi-level OUD stigma in rural North Carolina clinics and improve access to life-saving treatment.”
For those interested in learning more about the CNR Pilot Funding Program, check out the projects centered around cancer survivors and people living with HIV that were granted funding in Spring 2024.