School of Nursing Faculty Continue Fight Against Sickle Cell Disease
June 19 is World Sickle Cell Day. A number of Duke faculty continue to publish important research in the effort to mitigate the effects of the disease.
World Sickle Cell Day is a global event dedicated to raising awareness about sickle cell disease (SCD), a genetic blood disorder that affects millions worldwide. The United Nations General Assembly officially recognized this day to highlight the need for public education and to address the challenges faced by individuals with SCD and their families. Here at the Duke University School of Nursing, a number of faculty are engaged in vital research aimed at combating this debilitating disease.
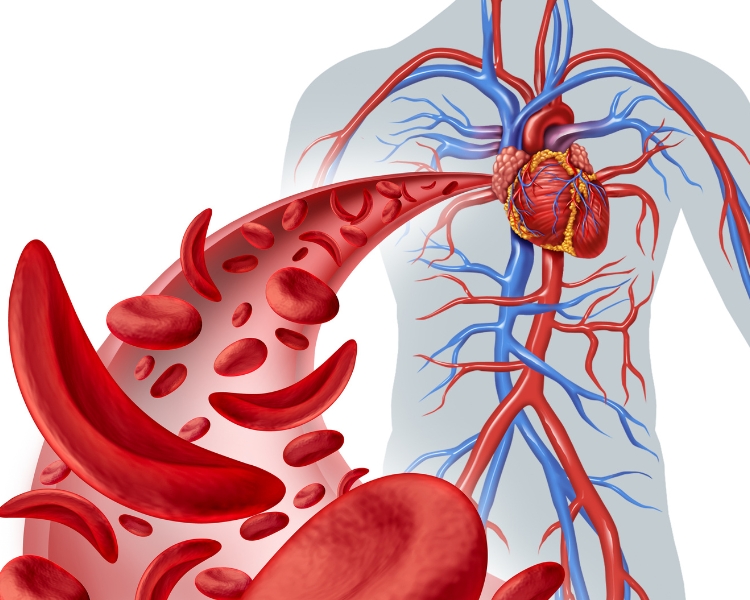
SCD is characterized by the production of abnormally shaped red blood cells that resemble a sickle. These cells can obstruct blood flow, leading to painful episodes known as sickle cell crises, organ damage, and other serious complications. The disease predominantly affects individuals of African and Caribbean descent but can occur in any ethnic group.
School of Nursing professors Paula Tanabe, PhD, RN, FAEN, FAAN and Susan G. Silva, PhD along with Hayden B. Bosworth, PhD, and Regina D. Crawford, MD of the Duke University School of Medicine, and other colleagues, recently published a study titled “Time to pain relief: A randomized controlled trial in the emergency department during vaso-occlusive episodes in sickle cell disease.” The study compared the effectiveness of individualized opioid protocols versus standard weight-based protocols for pain relief in sickle cell disease patients experiencing vaso-occlusive episodes (VOE) in emergency departments. Results indicated that individualized protocols led to more rapid and significant pain reduction, suggesting their potential to improve patient outcomes and emergency department efficiency.
Dr. Tanabe, along with Nancy Crego, PhD, RN, CHSE; Karen Reuter-Rice, PhD, NP, FCCM, FAAN; Audrey Blewer, PhD, MPH; and School of Nursing alumna La’Kita Knight, PhD, MSN, BS, RN, also published a SCD study in the journal Pediatric Blood & Cancer. The study examines the association between hydroxyurea (HU) adherence and transcranial Doppler (TCD) screenings in children with sickle cell disease (SCD) enrolled in North Carolina Medicaid. It found that children with better HU adherence and longer Medicaid enrollment had more TCD screenings, suggesting the need for interventions to improve evidence-based care. The prevalence of TCD screenings was low, indicating a gap in adherence to national guidelines for SCD management.
Lastly, Drs. Crego and Tanabe, along with School of Medicine colleague Dr. Nirmish Shah, published research in the Journal of Pediatric Hematology/Oncology that examines opioid prescription patterns among children and adults with Sickle Cell Disease (SCD) enrolled in North Carolina Medicaid, highlighting the impact of factors like age, sex, hydroxyurea adherence, and emergency department reliance on opioid use. The study revealed that a significant number of enrollees did not have opioid claims, with claims peaking at ages 18 to 30 and associated with longer Medicaid enrollment, male sex, and short-acting opioid prescriptions.
These three studies are just some of the work Duke School of Nursing faculty have produced in the fight against sickle cell disease. “Our faculty have a strong past and current portfolio of research and scholarship focused on improving health outcomes and quality of life for individuals living with SCD,” says Dr. Tanabe. “Nationally, DUSON has the largest number of nurse scientists with a program of research in SCD. Individuals with SCD are primarily Black, are negatively affected by several SDOH, and are often the victims of stigma and discrimination. They continue to experience a severely shortened lifespan and battle countless disease related complications.”
“Our faculty research team collects data to document the burden of SCD and lead interventions such as the use of complementary and integrative health therapies (e.g., acupuncture) to reduce pain,” she continues. “Our participation in the CDC Sickle Cell Data Collection program provides the data which has been used to lead health care policy changes in NC. Our efforts to disseminate and implement the SCD guidelines and decision support in NC have now expanded to the international community as we work to adapt and implement these resources in Nigerian healthcare facilities.”
The Duke School of Nursing SCD team includes Dr. Tanabe and Dr. Crego along with Mariam Kayle, PhD, RN, CCNS, FAAN; Stephanie Ibemere, PhD, RN; and Mitchell R. Knisley, PhD, RN, ACNS-BC, PMGT-BC.
The theme for World Sickle Cell Day 2024 is “Hope Through Progress: Advancing Care Globally.” This theme emphasizes the importance of medical advancements and the global effort to improve the quality of life for those living with SCD. It’s a call to action for researchers, healthcare providers, and policymakers to collaborate and drive progress in the management and treatment of this condition.
Despite the challenges, there is hope. Treatments like Hydroxyurea and blood transfusions have significantly improved the lives of many with SCD. As we observe World Sickle Cell Day, we are reminded of the resilience of those living with SCD and the ongoing efforts to enhance care and find a universal cure. It’s a day to stand in solidarity, spread knowledge, and ignite hope for a future where Sickle Cell Disease no longer poses a threat to health and well-being, and Duke University School of Nursing faculty and students continue to make important strides towards that future.
