Health Equity Reimagined
Solutions in Action: NEWS
Duke Grant Initiates Mental Health Collaboration Among East African Universities
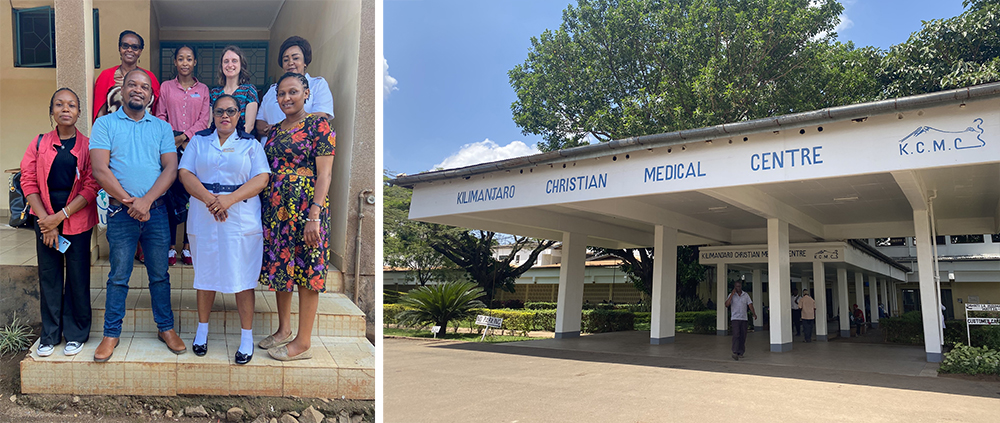
Duke University School of Nursing (DUSON) Assistant Professor Brandon Knettel, Ph.D., was recently awarded a grant by the Duke Global Health Institute (DGHI), where Knettel holds a secondary appointment as assistant research professor, to fund travel for East African scholars partnering with each other and Duke to impact mental health care in the region. The year-long grant will allow scholars from the University of Global Health Equity (UGHE) in Rwanda, Kilimanjaro Christian Medical Center (KCMC) in Tanzania, Moi University in Kenya, and Makerere University in Uganda to attend workshops at each of those institutions to learn about focused areas of expertise. The two-day workshops will include a combination of didactic training; visits to research and clinical sites to learn about existing services; collaborative planning for capacity building and funding opportunities; and professional networking.
Rwanda lost a million people to genocide in the 1990s, including many of the nation’s medically trained professionals. And in Tanzania, as recently as 2018, there were no psychiatrists or psychologists at KCMC, one of the largest hospitals in the country.
“Historically, mental health just hasn’t been a part of the health system and hasn’t been prioritized,” said Knettel, who has worked in Tanzania since 2009. But that is changing. The East African community has seen improvement in quality of life and fewer preventable deaths from things like malaria and HIV/AIDS, so now, mental health is the logical next step, Knettel said. But it needs support. The African and Duke scholars, who have begun collaborating with help from NIH grants, will work together not just to train new mental health care workers, but also to change how the care is delivered. The travel grant will facilitate that collaboration.
Inspired by the work of the late Paul Farmer, a Duke alumni and founder of UGHE in Rwanda, Knettel said these collaborative efforts among the four partner sites will build capacity in the region and address health inequities and social injustice.
“With a brand-new mental health system, we have the opportunity to reinvent the way health access works,” Knettel says. “It may be a lofty thing to say, but that’s really where we are.” Historically in other settings around the world, when introducing a new service, the people with the most resources get it first, Knettel said. “Here, we’re taking a different approach, where the people who need it most get it first.”
Brandon Knettel
PhD
One such program, led by Knettel and funded by the National Institute of Mental Health, focused on suicide prevention in Tanzania using a nurse-led strategy where three questions are added to a nurse’s patient inquiry. If patients’ responses to these mental health screening questions indicate they need further assessment, they can be seen immediately by a mental health provider via telehealth. If the patient agrees, they can then be directly connected to a mental health provider for treatment. Building the care into the existing system is not only cost-effective, it provides access to patients who might not ever seek help for serious mental distress. But catching more patients means more providers will be needed; supporting the local institutions in their training efforts is imperative to increasing capacity, a main goal of the partnership. “The need is so great that these providers, as soon as they come out of their training, they are just overwhelmed by the need already,” Knettel said.