Sickle Cell Disease Disproportionately Affects Black Community
Several faculty, staff devote time researching aspects of disease, its treatment.
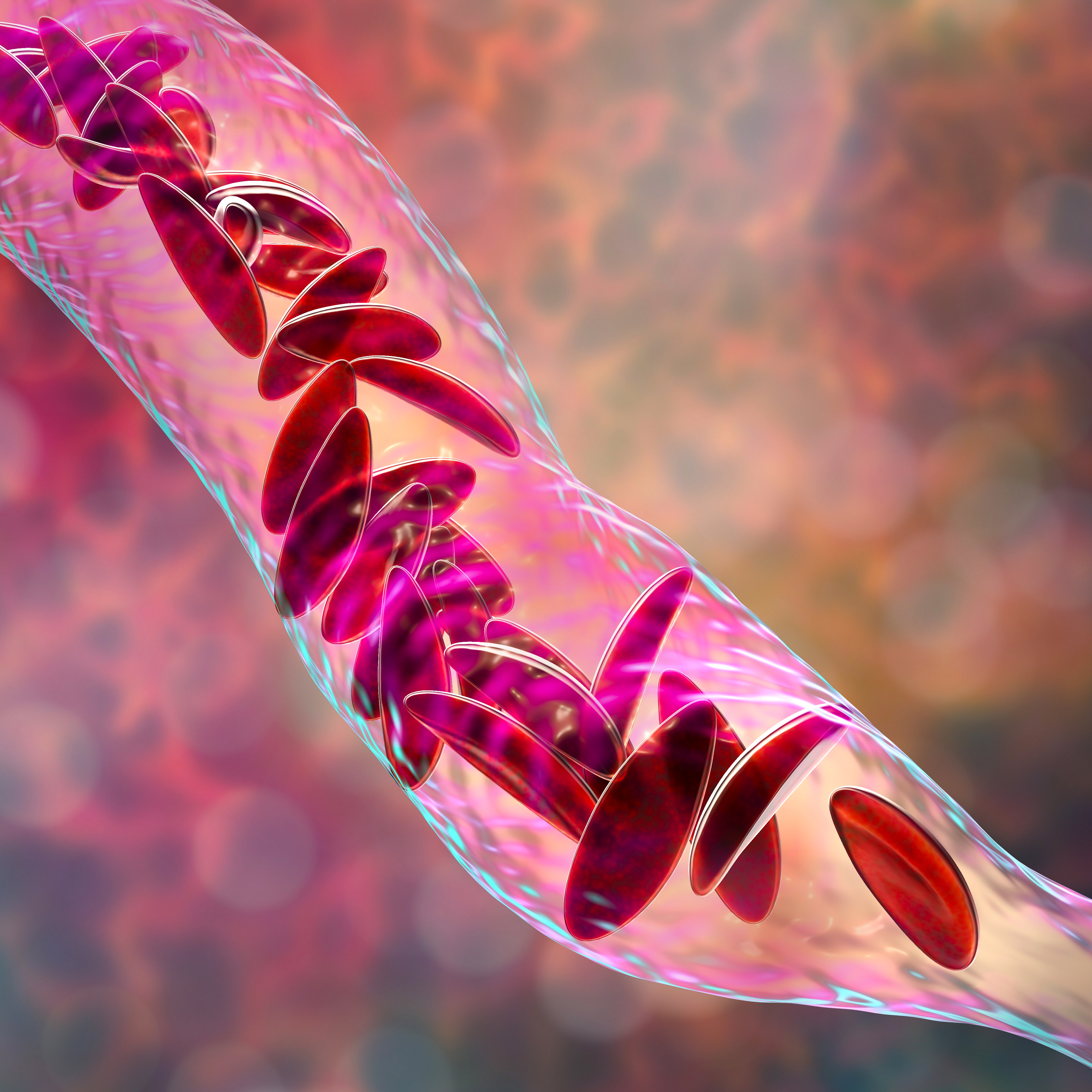
About 100,000 Americans live with sickle cell disease (SCD), according to the Centers for Disease Control and Prevention (CDC). One of every 365 of those Americans are of Black or African American births.
Numerous faculty and staff at the Duke University School of Nursing have made exploring SCD and the patients it affects a research priority.
 Dominique Bulgin
Dominique Bulgin
Dominique Bulgin, PhD ’19, consulting associate and postdoc fellow, has seen the ramifications of SCD firsthand, having friends and family who cope with the disease and having volunteered for a sickle cell clinic before starting nursing school, where she learned more about the nature of caring for SCD.
In 2020, she and her mentor, Paula Tanabe, PhD, MSN, MPH, RN, FAEN, FAAN, vice dean, Research, and Laurel Chadwick Professor of Nursing, received an award to pilot a telehealth personalized health planning program to improve SCD self-management, and in 2019, an article that she co-authored with Christian Douglas, consulting associate, and Tanabe that recapped a pilot test of two sickle cell-specific instruments was released in Pilot and Feasibility Studies.
 Nancy Crego
Nancy Crego
With an interest in health disparities, Nancy Crego, PhD, RN, CCRN, CHSE, assistant professor, has been involved with research on chronic pediatric illness and the influence of health care provider communication on disparities in care particularly on SCD patients. Last summer, she submitted a research application for a project that will aim to understand how COVID-19 has disproportionately affected health care utilization patterns for individuals with SCD in NC when compared to a sample of NC Medicaid enrollees without SCD. This follows her receiving an award in 2019 to explore the relationship of fetal hemoglobin responsiveness to hydroxyurea in adults with SCD.
 Stephanie Ibemere
Stephanie Ibemere
Stephanie Ibemere, postdoc fellow, published an article earlier this year with Jacqueline L. Brown, research program leader, and Tanabe on a trial design focused on comparing two protocols used to treat painful vaso-occlusive episodes, the most common reason patients with SCD visit the emergency room. Ibemere is also actively involved with building a research program focused in West Africa as a result of her dissertation research on the cultural influences on SCD management in Sierra Leone.
 Mariam Kayle
Mariam Kayle
Mariam Kayle, PhD, RN, CCNS, assistant professor, received an award in September entitled “North Carolina Sickle Cell Data Collection Program” to implement a high-quality state-wide, population-based SCD surveillance program in NC and then disseminate aggregate level reports to stakeholders and the CDC on the epidemiology and health care utilization patterns for SCD in NC. She met with congressional staff from November 30 to December 4 to discuss the program. She also co-authored "Impact of Medicaid expansion on access and healthcare among individuals with sickle cell disease" with Tanabe, which examined whether Medicaid expansion in California increased Medicaid enrollment, increased hydroxyurea prescriptions filled, and decreased acute healthcare utilization in SCD.
 Mitchell Knisely
Mitchell Knisely
Mitchell R Knisely PhD, RN, ACNS-BC, PMGT-BC, assistant professor, has shared several presentations on SCD. Last year, his presentations included "Pain Profiles in Sickle Cell Disease" at the Duke Center for Applied Genomics & Precision Medicine in January and "Patient-reported Outcomes in Sickle Cell Disease: Report from the SCDIC" at the National Institutes of Health for the Sickle Cell Disease Implementation Consortium Steering Committee meeting. In November, he presented on “Phenotypic Characterization and Genetics of Pain Profiles in Sickle Cell Disease” at the International Society of Nurses in Genetics (ISONG) 2020 World Congress; during that event, Robyn Wojeck, PhD student, won first place in the Student Poster Awards for her poster titled, “Genetic Polymorphisms and Pain in Sickle Cell Disease: A Systematic Review,” which Knisely co-authored. Earlier this month, Knisely discussed "Severe Pain Profiles in Patients with SCD: A Duke Report” at the NHLBI’s Sickle Cell Disease Implementation Consortium (SCDIC) Steering Committee Meeting; Eleanor Stevenson, chair of the Health of Women, Children & Families Division, spoke on "Fertility and infertility outcomes among females and males with sickle cell disease in the SCDIC registry” for that event.
He co-wrote an article with Rita Masese, associate in research, that evaluates pain impact, sleep impact, social functioning, depressive symptoms, tiredness, and cognitive function and identifies associated demographic and clinical characteristics of individuals with SCD. In October, he submitted an application with Allison Ashley-Koch of Duke Molecular Physiology Institute on a cross-sectional study to look at the epigenetic age acceleration and psychoneurological symptoms in SCD.
 Rita Masese
Rita Masese
In addition to the article she co-wrote with Knisely, Masese is the leading author of “Effective Recruitment Strategies for a Sickle Cell Patient Registry Across Sites from the Sickle Cell Disease Implementation Consortium (SCDIC)” in the Journal of Immigrant and Minority Health. The article analyzes the recruitment strategies and challenges of SCD Implementation Consortium. Majority of the study’s participants were African American.
Masese’s study was covered in HCPLive.
 Paula Tanabe
Paula Tanabe
Tanabe is a sickle cell expert, with her program of research focused on improving systems of health care and patient outcomes for people with SCD, specifically regarding the advancement of their patient care. She has written and co-authored numerous articles, including ones co-written with Bulgin, Ibemere and Kayle. Last June, she and Crego submitted an application to better understand how COVID-19 has changed SCD management, examining emergency department visits, in-patient stays, ambulatory visits, and the use of telephone and telehealth visits as well as prescribing patterns for hydroxurea and opioids.
In 2019, Tanabe experienced what she deemed at that time “the highlight of my career.” Tanabe had spent more than a decade of research, planning and advocacy with colleagues in NC and throughout the US to help patients with SCD receive treatment for severe pain in the emergency department. In September 2019, her and her colleagues’ hard work reached a climatic point when the General Assembly of the Emergency Nurses Association voted to adopt a resolution, drafted by Tanabe and two other emergency department nurses from North Carolina, to disseminate evidence-based guidelines and education on sickle cell treatment to all emergency departments in the United States.